Successful treatment of childhood OCD (obsessive-compulsive disorder) is associated with an increase of quality of life in the long term. This was demonstrated by a new study, published by first author Sanne Jensen, the NordLOTS group and me as a co-author. This study is a long-term follow up of one of the largest pediatric OCD studies, the Nordic Longterm OCD Treatment Study (NordLOTS), conducted in Denmark, Norway and Sweden: 220 children 7 to 17 years received CBT in a first step (cognitive behavior therapy). Those who did not respond fully to CBT received either more CBT or medication (a so called SSRI, selective serotonin reuptake inhibitor).
The children’s quality of life was rated by themselves and their parents during treatment, and yearly for 3 years after completed treatment. The results show that children who responded to treatment directly did also simultaneously experience a marked increase in quality of life. Those who responded in a more gradual manner over time or with a limited response also improved in quality of life, but only on the parent ratings.
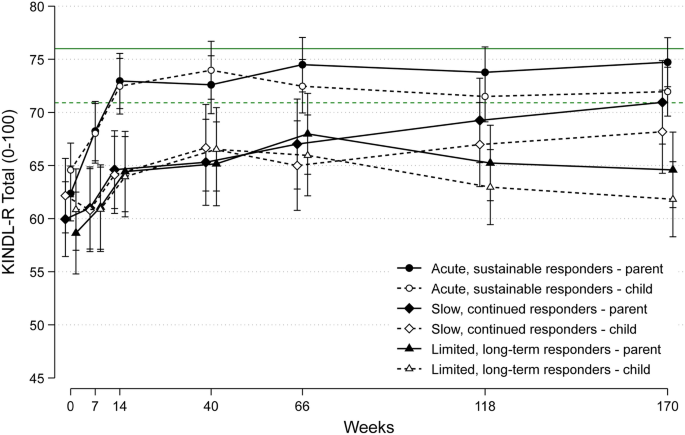
This study is one of the very few long-term follow ups on the effect of OCD treatment on quality of life in youth. The results are encouraging and show that quality of life returns to normal levels once the OCD is treated properly with evidence-based treatments.
References
Sanne Jensen, Katja A. Hybel, Davíð R. M. A. Højgaard, Judith Becker Nissen, Bernhard Weidle, Tord Ivarsson, Gudmundur Skarphedinsson, Karin Melin, Nor Christian Torp, Anders Helles Carlsen, Erik Lykke Mortensen, Fabian Lenhard, Scott Compton & Per Hove Thomsen. Quality of life in pediatric patients with obsessive–compulsive disorder during and 3 years after stepped-care treatment. Eur Child Adolesc Psychiatry (2021). https://doi.org/10.1007/s00787-021-01775-w
This study is part of the NordLOTS project. The two main outcomes papers are referenced below. The step 1 outcome paper presents results from 14 weeks of CBT. Step 2 presents the results of CBT non-responders when randomized to additional CBT or SSRI.
Torp NC, Dahl K, Skarphedinsson G et al (2015) Effectiveness of cognitive behavior treatment for pediatric obsessive-compulsive disorder: acute outcomes from the Nordic Long-term OCD Treatment Study (NordLOTS). Behav Res Ther 64:15–23. https://doi.org/10.1016/j.brat.2014.11.005
Skarphedinsson G, Weidle B, Thomsen PH et al (2015) Continued cognitive-behavior therapy versus sertraline for children and adolescents with obsessive-compulsive disorder that were non-responders to cognitive-behavior therapy: a randomized controlled trial. Eur Child Adolesc Psychiatry 24:591–602.https://doi.org/10.1007/s00787-014-0613-0